Monkeypox, a rare but concerning viral disease, has recently gained international awareness due to several outbreaks. In this graphical direction, we’ll carry you via the necessary elements of the Monkeypox outbreak, presenting a clear understanding of the disease through compelling images and sketches. From the virus’s sources and symptoms to its spread and prevention, these visuals will help you learn the basic facts at a glance. Whether you want to educate yourself or others, these insights will provide a comprehensive look at Monkeypox and its effects.
Monkeypox pictures






Key facts:
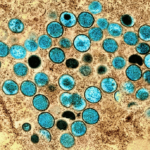
- Mpox, also known as monkeypox, is a viral illness caused by the monkeypox virus, which belongs to the Orthopoxvirus family. This virus has two main types: clade I and clade II.
- Common mpox symptoms include a skin rash or sores in the mouth and other mucous areas, lasting 2 to 4 weeks. Fever, headache, muscle aches, back pain, fatigue, and swollen lymph nodes often accompany these symptoms.
- Mpox spreads to humans through close contact with an infected person, contaminated objects, or infected animals.
- Mpox is confirmed in the lab by testing samples from skin lesions using a PCR test.
- Mpox is treated with supportive care, and in some cases, smallpox vaccines and treatments—approved for use in specific countries—can also help manage the mpox.
- Between 2022 and 2023, a worldwide mpox outbreak was driven by a specific strain called clade IIb.
- You can prevent mpox by avoiding close contact with anyone with the disease. Vaccination can also help protect those at higher risk of infection.
For more in-depth information, visit the WHO’s official page at this link.
What Is Monkeypox?
Monkeypox is a periodic viral infection comparable to smallpox but usually less painful. It was first discovered in monkeys, which is how it got its name, but the virus can also infect humans. The disease is mainly found in small parts of Central and West Africa, frequently around tropical rainforests.
Before 2022, most cases of mpox appeared in central and western Africa. However, cases of mpox caused by the West African form of the virus have been reported in 94 countries. Trusted Source worldwide as of this article’s publication, including in locations where it doesn’t usually appear.
Keep reading to understand why mpox happens, what symptoms to look for, and how it’s diagnosed. This article will also explain how mpox spreads and how it can be treated.
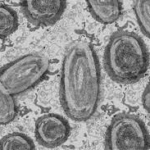
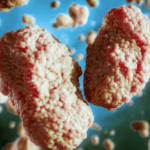
What is the cause of monkeypox?
The Monkeypox virus causes monkeypox, a component of the Orthopoxvirus genus, including the smallpox virus. The virus primarily spreads in animals like rodents and primates in Central and West Africa, and it can occasionally jump to humans. People can acquire monkeypox via immediate touch with an infected animal, such as through a bite or scratch or by taking the animal’s body fluids or lesions. In certain situations, Monkeypox can spread from person to person through close contact, respiratory droplets, or by touching infected items such as bedding or clothing. While the virus equals smallpox, it’s usually less contagious and painful.
What Are the Symptoms of Monkeypox?
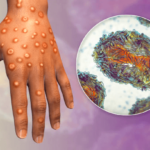
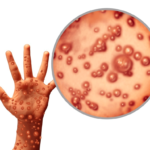
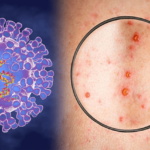
Monkeypox generally starts with flu-like signs such as fever, headache, muscle pains, and tiredness. These earlier signs are usually attended by swollen lymph nodes, which can help determine Monkeypox from similar diseases like smallpox. A few days after the fever begins, a rash develops, usually starting on the face and then spreading to other body parts, including the palms of the hands and soles of the feet.
The rash goes via various stages, starting with flat spots, raised bumps, fluid-filled blisters, and scabs that eventually fall off. The entire infection usually lasts 2 to 4 weeks, and while most people recover completely, the rash can be painful and may leave scars. Identify these signs early and seek medical guidance if you suspect an infection is required.
The early symptoms can contain:
- Fever, which is usually the first sign
- Headache
- Muscle Pains
- Backache
- Fatigue
- Coolness
- Swollen lymph nodes, also known as lymphadenopathy
After the fever evolves, a rash usually occurs 1 to 3 days later.
The rash generally impacts your:
- Face, which is the most common site
- Palms of your hands
- Soles of your feet
- Mouth
- Genitalia
- Eyes, including the conjunctivae and cornea
A rash may appear before or behind the madness and further flu-like signs; some people may experience a rash.
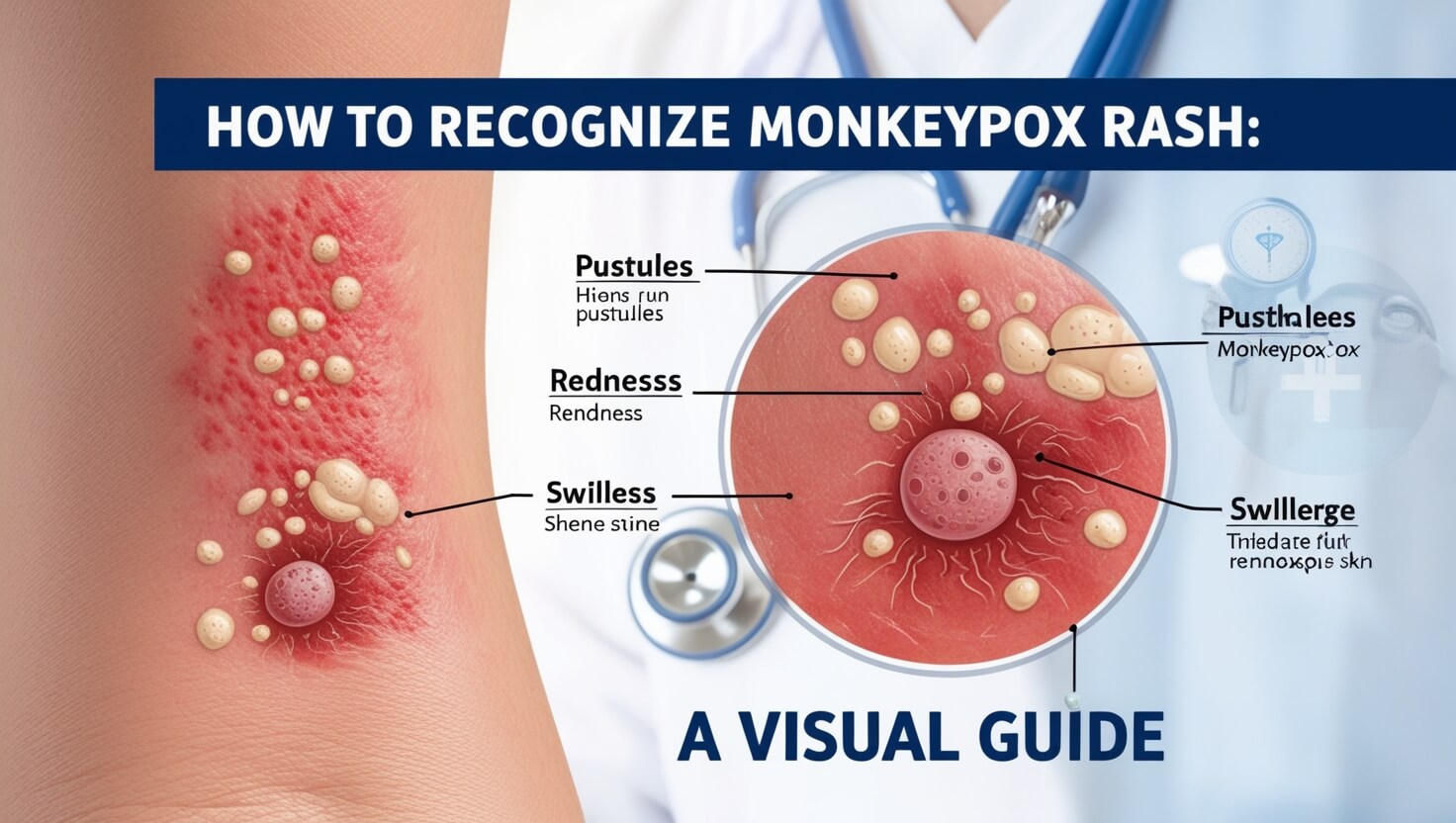
The mpox rash starts with lesions that change through these stages:
- Macules, or flat, discolored lesions
- Pimples or slightly increased lesions
- Vesicles, or pimples with transparent liquid
- Pustules, or pimples with yellowish liquid
- Scabs
After the lesions dry and scab over, they drop off. The mpox signs generally last 2 to 4 weeks and reach out without medicine.
How Does Monkeypox Spread?
Monkeypox extends via close connection with an infected person or animal. The virus can be transferred from animals to humans when someone is bitten or scratched by an infected animal or by taking animals or animal products like meat and skin. Monkeypox can spread to individuals through immediate contact with physical fluids, respiratory droplets, or skin sores of an infected person. It can also spread by touching infected surfaces or objects, like bedding or clothes. Although person-to-person transmission is ordinary, handling protection is still essential, particularly in places where the virus is known to be present.
Mypox spreads through direct touch with the mpox virus through the following importance:
- Blood
- Bodily liquids
- Skin or mucous lesions
- Respiratory droplets for human-to-human touch
It can also spread through connection with objects, clothes, or surfaces, including the mpox virus. People who are pregnant can also pass the virus to their fetus via the placenta.
According to the Centers for Disease Control and Prevention (CDC)Trusted Source, the mpox virus can also be extended through close contact, which contains:
- Hugging, massaging, or kissing
- Oral, anal, or vaginal relations
- Connecting the genitals or anus of someone with the mpox virus
- Prolonged face-to-face connection
- Touching entities during sex that include the mpox virus, such as bedding, towels, or sex toys
Information can also occur around:
- Bites and scratches from creatures with a mpox disease
- Eating the meat of a beast with a mpox disorder
Possible complications that can arise from having Monkeypox.
While monkeypox is commonly a self-limiting infection, representing most individuals rescued without severe cases, it can cause difficulties, particularly in typical individuals. Potential challenges include secondary bacterial disorders of the skin, respiratory troubles, and, in some possibilities, eye disorders that can lead to vision loss. The infection can become more intense for people with tired immune systems, leading to difficulties like pneumonia, sepsis, and encephalitis, which is brain inflammation. Observing signs near and pursuing medical care if the sickness worsens is required, as before treatment can help control these difficulties.
Likely difficulties of mpox contain:
- Bronchopneumonia
- Sepsis
- Inflammation of brain tissue, also known as encephalitis
- Disease of the cornea, the transparent farthermost coating of your eye
- Secondary diseases
A disease in the cornea may lead to vision loss. In extreme circumstances, the lesion’s strength combines. This may cause the failure of an extensive range of skin.
Where is monkeypox commonly found?
Monkeypox is primarily discovered in small parts of Central and West Africa, especially in regions near tropical rainforests. The infection is standard in nations like the Democratic Republic of the Congo, Nigeria, and Cameroon. While it was initially restricted to these zones, occasional outbreaks have been reported in additional parts of the globe, usually linked to journeys or the importation of animals. The virus commonly extends from beasts, such as rodents or primates, to humans, making hotspots for the sickness in these regions, where people live near wildlife.
Historically, the mpox virus was especially active in tropical, rural regions of central and western Africa. Since 1970Trusted Authority has occurred in the following nations:
- Benin
- Cameroon
- Central African Republic
- Cote d’Ivoire
- Democratic Republic of the Congo
- Gabon
- Liberia
- Nigeria
- Republic of the Congo
- Sierra Leone
- South Sudan
Historically, most reported cases of mpox are from rural regions of the Democratic Republic of the Congo.
However, as of August 2022, cases of mpox have been noted in 87 different countriesTrusted Source. Where the virus doesn’t usually happen, with 39,434 entire topics noted worldwide.
Also, on July 23, 2022, the World Health Organization (WHO)Trusted Source officially announced the mpox outbreak as a Public Health Emergency of International Concern.
Does monkeypox pose a risk of death?
Monkeypox is generally not as harmful as other viral diseases but can still be serious, especially in specific populations. Most people contracting Monkeypox experience flu-like signs and a rash that is usually removed within a few weeks. However, in rare circumstances, specifically in people with tired immune systems, young youths, or those in zones with limited entry to healthcare, Monkeypox can lead to severe difficulties and even death.
The mortality rate varies depending on the tune, with some strains being more risky than others. While taking Monkeypox is essential, most people can fully recover with suitable medical supervision.
Certain people may be better sensitive to extreme sickness and difficulties, including:
- People with tired immune systems
- Youngsters under eight years old
- Someones who are pregnant or breastfeeding
- People with a history of eczema
Some people who experience secondary bacterial disorders tend to have worse results.
Monkeypox Cases in the U.S. During 2022
In 2022, the United States faced a compelling wave of Monkeypox cases, turning what was once a periodic and relatively unrecognized disease into a significant public health case. Once restricted to specific areas, the virus started circulating nationally, prompting widespread problems and movement from health management. Monkeypox, equal to smallpox but typically less painful, spreads primarily via close biological connection with an infected person or animal, causing it specifically to be involved in settings where people are nearby.
As cases increased, health administrators ramped up vaccination campaigns, specifically targeting individuals at higher risk of disease, such as healthcare employees and those in close touch with infected people. General health announcements highlighted the significance of identifying signs before, seeking prompt medical supervision, and handling preventative measures to decrease the risk of spreading the virus.
As of August 17, 2022, 39,434 cases of Trusted Source have been registered worldwide in 94 different nations. This contains 13,517 cases of rusted Sources in the United States, with the most increased number of cases appearing in:
- New York
- California
- Florida
- Texas
- Georgia
On August 4, 2022, mpox was announced as a general health crisis in the United States.
How is Monkeypox Treated?
Monkeypox therapy mainly reduces signs and supports the patient as their body fights off the virus. There is no exact antiviral therapy for Monkeypox, so care usually concerns controlling fever, pain, and discomfort with medicines and quantity of leaves. In additional severe cases, medical experts may use antiviral medications that are also useful against smallpox. Securing a patient remains hydrated and bypassing secondary infections is also significant.
For those at a more increased risk of difficulties, such as those with weakened immune systems, healthcare providers strength present extra treatments to help control the disease. While there is no one-size-fits-all treatment, supportive supervision can help patients recover comfortably.
Some medications can control an outbreak and prevent the infection from spreading. They can contain:
- Vaccinia vaccine (smallpox vaccine)
- Vaccinia immune globulin
- Antiviral medicine (in beasts)
- Tecovirimat (TPOXX), an antiviral used to treat smallpox
- Brincidofovir (Tembexa) is an antiviral medication utilized to treat both adults and youths with smallpox.
- Cidofovir, which is generally used to treat eye infections caused by cytomegalovirus but has been used in specific mpox cases
Can getting vaccinated protect you from monkeypox?
Yes, vaccination can help prevent Monkeypox. The smallpox vaccine, operated for decades to defend against the smallpox virus, has also provided an effective shield against Monkeypox. This is because the two viruses are closely connected. While Monkeypox is more infrequent and less potent than smallpox, the vaccine can always decrease the chance of disease. Health management may suggest vaccination during attacks, mainly for those at higher exposure risk. If you’re concerned about Monkeypox or believe you might be at risk, speaking to a healthcare provider concerning vaccination can be an aggressive step to save your fitness.
The WHO declares that the smallpox vaccine is almost 85% useful in assisting in controlling mpox. If you acquired the smallpox vaccine as a kid and contracted the mpox virus, your symptoms may be mild. Nowadays, the CDC Trusted Source suggests vaccination for someone exposed to mpox and those at an increased chance of acquiring the virus.
This contains people who:
- Have been determined by public health officials as a close connection of someone with mpox
- Have had a sexual partner within the past two weeks who’s been analyzed with mpox
- Have had multiple sexual partners within the past two weeks in a location where mpox cases have been noted
- Who has a job that discloses them to orthopoxviruses, including mpox
In addition to acquiring vaccination, the CDC recommends Trusted sources wash their hands repeatedly and avoid immediate connection with people with mpox or objects they might’ve used to control the disease.
Who should get screened for monkeypox, and how is it diagnosed?
Filtering for Monkeypox is essential for those who have been in close connection with a person diagnosed with the infection or who have just traveled to places where Monkeypox is known to ensue. Pursuing medical advice is crucial if you experience symptoms such as fever, headache, muscle pains, and a distinctive rash. The diagnosis typically affects a healthcare provider who reviews your signs and medical record and verifies the existence of the virus via laboratory tests. These tests can catch the virus’s genetic fabric or proteins in samples carried from skin lesions or further physical liquids. Early detection and diagnosis are essential to effectively operating Monkeypox and controlling its spread.
Physicians analyze Source mpox in several ways:
Lab trials: This involves trying the liquid from lesions or dry scabs. A polymerase chain reaction (PCR) trial can review these samples for the virus.
Biopsy: A biopsy involves removing a piece of skin tissue and trying it for the virus.
Blood tests aren’t usually suggested. That’s because the mpox virus remains in the blood shortly. Thus, it’s not an authentic trial for analyzing mpox.
If you want to learn more articles on topics you are interested in, you can visit our website. https://dailyexploreusa.com/
FAQ
Is Monkeypox currently present in the US?
Yes, Monkeypox (mpox) has been reported in the US. Cases have occurred in different states, prompting health administrators to observe and handle the circumstances closely.
Why did WHO declare mpox a global health emergency?
The World Health Organization announced Monkeypox as a global health crisis due to its quick spread, an unusual digit of cases in non-endemic countries, and the possibility of crucial public health effects.
Is there a chance that mpox will lead to another lockdown?
It is doubtful that Monkeypox will cause another lockdown. Public health measures concentrate on preventing the spread of the virus via vaccination, therapy, and isolation instead of overall lockdowns.
How to Prevent Mpox
Controlling Monkeypox affects:
- Avoid contact with infected people or animals.
- Rehearsing suitable hygiene.
- Utilize protecting actions if you’re in high-risk atmospheres.
Vaccination can also supply security.
What are the main symptoms of Monkeypox?
The major symptoms of Monkeypox contain flu-like signs such as fever, headache, muscle pains, and tiredness, observed by a specific rash that progresses through several steps: macules, papules, vesicles, pustules, and scabs.
How can I determine if a rash is Monkeypox?
To recognize a Monkeypox rash, look for the advance from flat pink spots to increased pimples, fluid-filled blisters, and pus-filled bumps. The rash is in different stages simultaneously. Consulting a healthcare provider is necessary for a definitive diagnosis.
Are there any current updates or unique analyses on how to determine Monkeypox?
Yes, recent investigations are constantly occurring to enhance the identification and diagnosis of Monkeypox. Advances in diagnostic tests and knowledge of the virus help better detect and supervise the infection.
What should I do if my Monkeypox rash is healing but new spots keep showing up?
If new lesions arise while existing ones heal, consult a healthcare provider. This could suggest continuing disease or difficulties that require medical evaluation and control.
How can I manage Monkeypox lesions to prevent spreading the virus?
Control Monkeypox lesions carefully by avoiding connecting or scratching them. Clean your hands often, protect the lesions with hygienic applications, and keep proper hygiene to control the spreading of the virus.
What are the treatment options for Monkeypox rash?
Monkeypox has no specific therapy, but supporting supervision can help control symptoms. Over-the-counter medications, such as silicone scar sheets and ointments, can help with scar control. Consult a healthcare provider for suitable supervision.
Can Monkeypox rash appear in hard-to-see areas?
Yes, Monkeypox rash can begin in small visual places, such as inside the mouth or genital regions, making earlier detection more demanding. It is important to seek medical guidance if you suspect monkeypox or if the rash is not clearly observable.
What should I do if I’m unsure whether my rash is Monkeypox?
If you’re uncertain whether your rash is Monkeypox and has been disclosed to conceivable authorities, consult a healthcare provider. Virtual talks with dermatologists suggest immediate reviews and suggestions.